Reflux after gastric sleeve surgery is a common concern for many patients, especially during the early recovery phase. While gastric sleeve surgery in Melbourne has become a popular and effective option for weight loss, it can sometimes increase acid reflux symptoms as your stomach heals and adjusts to its new shape. With the right dietary habits, you can significantly reduce discomfort and support long-term recovery
This guide by Dr. Niruben Rajasangram explains why reflux may happen, how long it lasts, and most importantly, the practical diet tips you can follow to keep symptoms under control. If you are wondering, “does acid reflux go away after gastric sleeve surgery?”, the answer depends on consistent surgery performed, lifestyle adjustments, starting with what and how you eat.
Why Reflux Happens After Gastric Sleeve Surgery
Reflux after gastric sleeve surgery occurs mainly because the stomach becomes smaller and narrower. This change can increase internal pressure, making acid more likely to move upwards. Additionally, the healing process temporarily weakens the valve between the stomach and oesophagus.The more likely reason for reflux happening post gastric sleeve surgery is that the lack of repairing the anti-reflux valve at the time of the gastric sleeve surgery. Mr Niruben always assess the hiatus which forms part of the antireflux valve as it has frequently been found that even when a patient has no reflux symptoms prior to surgery. There is already a natural weakness of this valve. Failing to address this will see intra-thoracic migration of the sleeved stomach and the presence of reflux.
Common symptoms include:
-
Burning sensation in the chest
-
Regurgitation or sour taste
-
Bloating or discomfort after meals
-
Feeling overly full quickly
While these symptoms are uncomfortable, they usually improve with the right eating habits. Many patients also ask, “How long does acid reflux last after gastric sleeve surgery?” for most, symptoms settle within weeks to months, depending on individual healing and diet choices.
If you’re still in the decision-making stage or want a clearer understanding of whether this procedure fits your health goals, you can explore more details in our related guide: Is Gastric Sleeve Surgery Right for You? A Surgeon’s Perspective.
Best Diet Tips to Control Reflux After Gastric Sleeve Surgery
The following dietary strategies are proven to reduce reflux after gastric sleeve surgery and support long-term digestive comfort.
1. Eat Smaller, More Frequent Meals
One of the simplest but most effective ways to control reflux is to eat in smaller portions. Overfilling the reduced stomach can create immediate pressure that pushes acid upward.
Why it works:
The narrower stomach after surgery cannot handle large amounts of food at once. Controlled portions reduce discomfort and support smoother digestion.
Tip: Aim for 4–6 small meals spaced throughout the day.
2. Chew Food Thoroughly and Eat Slowly
Eating too quickly is a leading trigger of reflux after gastric sleeve surgery. Proper chewing helps break down food before it reaches the stomach, making digestion easier and reducing unnecessary strain.
Tip: Put your fork down between bites and take at least 20–25 minutes to finish a meal.
3. Avoid Trigger Foods That Increase Acid Production
Some foods naturally cause the stomach to produce more acid or relax the lower oesophageal sphincter, the muscle that keeps acid where it belongs.
Common triggers include:
-
Spicy foods
-
Tomato-based sauces
-
Citrus fruits
-
Garlic and onions
-
Coffee and caffeinated beverages
-
Chocolate
-
Mint
-
Fried or greasy foods
Eliminating these foods in the early months can significantly reduce symptoms.
4. Choose Low-Acid, Gentle Foods
After surgery, your digestive system is sensitive. Low-acid, easily digestible foods reduce irritation and help the stomach heal.
Examples include:
-
Lean proteins like chicken, turkey, tofu, and white fish
-
Plain yoghurt
-
Oats, whole grains, and soft vegetables
-
Bananas, melons, and applesauce
These foods help soothe the stomach rather than stimulate acid.
5. Stay Upright After Eating
Lying down soon after meals increases the chance of reflux after gastric sleeve surgery. Gravity helps keep acid in the stomach, so staying upright supports natural digestion.
Tip: Wait at least 45–60 minutes before lying down or reclining.
6. Limit Fluids During Meals
Drinking large amounts of fluid with food can overwhelm the stomach and contribute to reflux symptoms.
Tip: Sip fluids throughout the day, but avoid drinking 20–30 minutes before or after meals.
7. Avoid Carbonated Beverages
Carbonation increases pressure inside the stomach, which can worsen reflux and cause discomfort. This is especially important during the first year after surgery.
Choose still water, herbal teas, or doctor-approved hydration alternatives instead.
8. Include Lean Protein in Every Meal
Protein is essential for healing after bariatric procedures, and it helps stabilise digestion. However, the type of protein matters.
Opt for soft, lean, and moist protein sources that are gentle on your stomach. Avoid fried or heavily seasoned options.
9. Maintain a Balanced Eating Schedule
Skipping meals or overeating at one time can trigger reflux after gastric sleeve surgery. A consistent schedule allows the stomach to process food gradually and keeps acid production stable.
10. Pay Attention to Food Textures During Early Recovery
During the first few phases after surgery, the liquid, puree, and soft food stages, following guidelines strictly helps reduce reflux. Dense or dry foods may be difficult to tolerate early on.
Introduce new textures slowly and monitor how your body responds.
11. Keep a Food Diary to Identify Patterns
Not everyone has the same reflux triggers. Tracking what you eat and how you feel afterwards helps identify problem foods unique to your body.
This simple habit makes diet adjustments more effective.
12. Seek Guidance from a Bariatric Specialist
If reflux symptoms persist beyond the expected recovery time, consulting a bariatric specialist can help. They may review your dietary habits, check for underlying issues, or assess whether GERD surgery is required for severe cases. Most patients do not require additional surgery, but professional evaluation is a valuable step for long-term comfort.
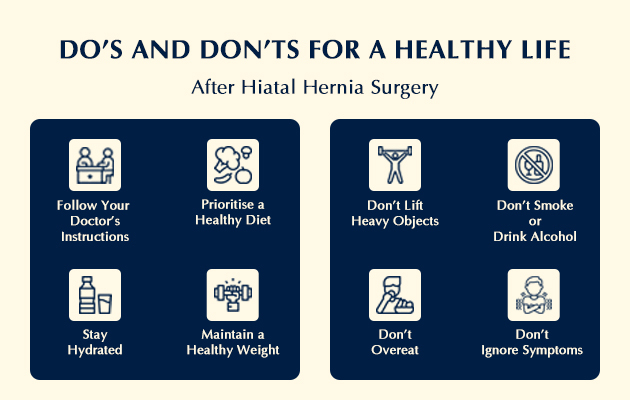
Lifestyle Habits That Support Digestive Recovery
Diet plays a major role, but lifestyle habits also help reduce symptoms of reflux after gastric sleeve surgery.
Maintain a Healthy Weight
Weight loss after surgery gradually reduces abdominal pressure, which in turn eases reflux. As weight decreases, patients often notice that reflux becomes less frequent.
Sleep With Your Upper Body Elevated
Raising the head of your bed by 15–20 cm or using wedge pillows helps keep stomach acid down while sleeping. This is particularly helpful during the early recovery stages.
Follow Up With Your Bariatric Specialist
If reflux persists longer than expected, your bariatric specialist may adjust your diet, medication, or lifestyle plan. In some cases, patients may require evaluation for GERD surgery in Melbourne, especially if symptoms do not improve with standard management. Regular follow-ups ensure that any concerns are addressed early.
When Does Reflux Improve After Gastric Sleeve Surgery?
For most people:
-
Mild reflux settles within a few weeks.
-
Moderate reflux may last for a few months.
-
Persistent reflux should be assessed by a bariatric specialist to rule out underlying issues.
Following a structured diet and lifestyle plan significantly shortens the duration and intensity of reflux after gastric sleeve surgery.
|
Note: These recommendations are general guidelines and may not be suitable for everyone. Before making any dietary or lifestyle changes, it is always best to consult a bariatric specialist or healthcare provider for personalised advice tailored to your recovery. |
Why Choose Niruben Rajasangram?
Choosing the right bariatric specialist plays an important role in managing reflux after gastric sleeve surgery and ensuring long-term digestive comfort. Under the care of Niruben Rajasangram, patients receive guidance that goes beyond the procedure itself. His approach focuses on understanding each patient’s symptoms, recovery timeline, and food tolerance levels to help them manage concerns such as reflux more effectively. He always assess the hiatus which forms part of the antireflux valve as he has frequently been found that even when a patient has no reflux symptoms prior to surgery there is already a natural weakness that needs to be addressed surgically.
What makes his care particularly helpful is the emphasis on:
-
Personalised post-surgery support: Every patient’s digestive system adapts differently after a sleeve gastrectomy. You receive personalised dietary advice and symptom-management strategies based on your individual needs.
-
Evidence-based recommendations: Instead of generic advice, you are guided with practical, clinically supported strategies designed to reduce reflux and improve recovery.
-
Focus on long-term outcomes: Managing reflux is not just about early recovery. The goal is to help you build sustainable eating habits that support your health months and years after surgery.
-
Clear communication: You’ll understand what to expect, how long symptoms may last, and what steps to take if reflux continues. This helps reduce confusion and empowers you to manage your recovery confidently.
With this patient-centred approach, you receive the reassurance, clarity, and structured guidance needed to control reflux effectively after gastric sleeve surgery while supporting a healthier long-term lifestyle.
For patients who experience ongoing reflux or want to understand advanced treatment options, you may also find our detailed guide helpful: Understanding Anti-Reflux Surgery: What Patients Can Expect and How to Prepare.
Take Away
Reflux after gastric sleeve surgery is common, especially in the early phase of recovery, but it can be managed effectively with the right diet and habits. Eating smaller meals, avoiding trigger foods, staying upright after eating, choosing low-acidity options, and following structured nutritional guidelines all play a key role in reducing discomfort. Most patients find that reflux improves as the stomach heals, but tracking your symptoms and working closely with your bariatric specialist ensures safer, smoother progress.
With consistent care and the right dietary approach, you can regain comfort, support healthy digestion, and continue your recovery with confidence after gastric sleeve surgery in Melbourne under the guidance of Niruben Rajasagaram
Frequently Asked Questions
Can gastric sleeve surgery cause reflux even if I never had it before?
Yes, some patients experience reflux for the first time after gastric sleeve surgery because the stomach shape changes and internal pressure temporarily increases. This is usually temporary and improves with proper diet and healing.
Does reflux mean my gastric sleeve surgery was unsuccessful?
No, reflux alone is not an indicator of an unsuccessful surgery. It is a common part of the healing process. Most patients experience significant improvement with dietary adjustments, weight loss, and follow-up care.
Will medications help manage reflux after gastric sleeve surgery?
Many patients benefit from short-term use of acid-reducing medications prescribed by their specialist. These medications help protect the healing stomach and reduce discomfort. Always follow medical guidance before using them.
Can stress or poor sleep make reflux worse after surgery?
Yes, stress and irregular sleep patterns can increase acid production and slow digestion, which may worsen reflux. Relaxation techniques, good sleep posture, and a consistent routine can support recovery.
Is it safe to exercise while experiencing reflux after gastric sleeve surgery?
Light exercise, such as walking, is safe and can actually improve digestion. However, avoid high-intensity workouts or movements that compress the abdomen right after meals, as these may increase reflux symptoms.
Can long-term reflux lead to complications after gastric sleeve surgery?
If left unmanaged, chronic reflux can irritate the oesophagus. This is why regular follow-ups with your bariatric specialist are essential. Early intervention ensures symptoms don’t progress and keeps your digestive health protected.